About LSARC
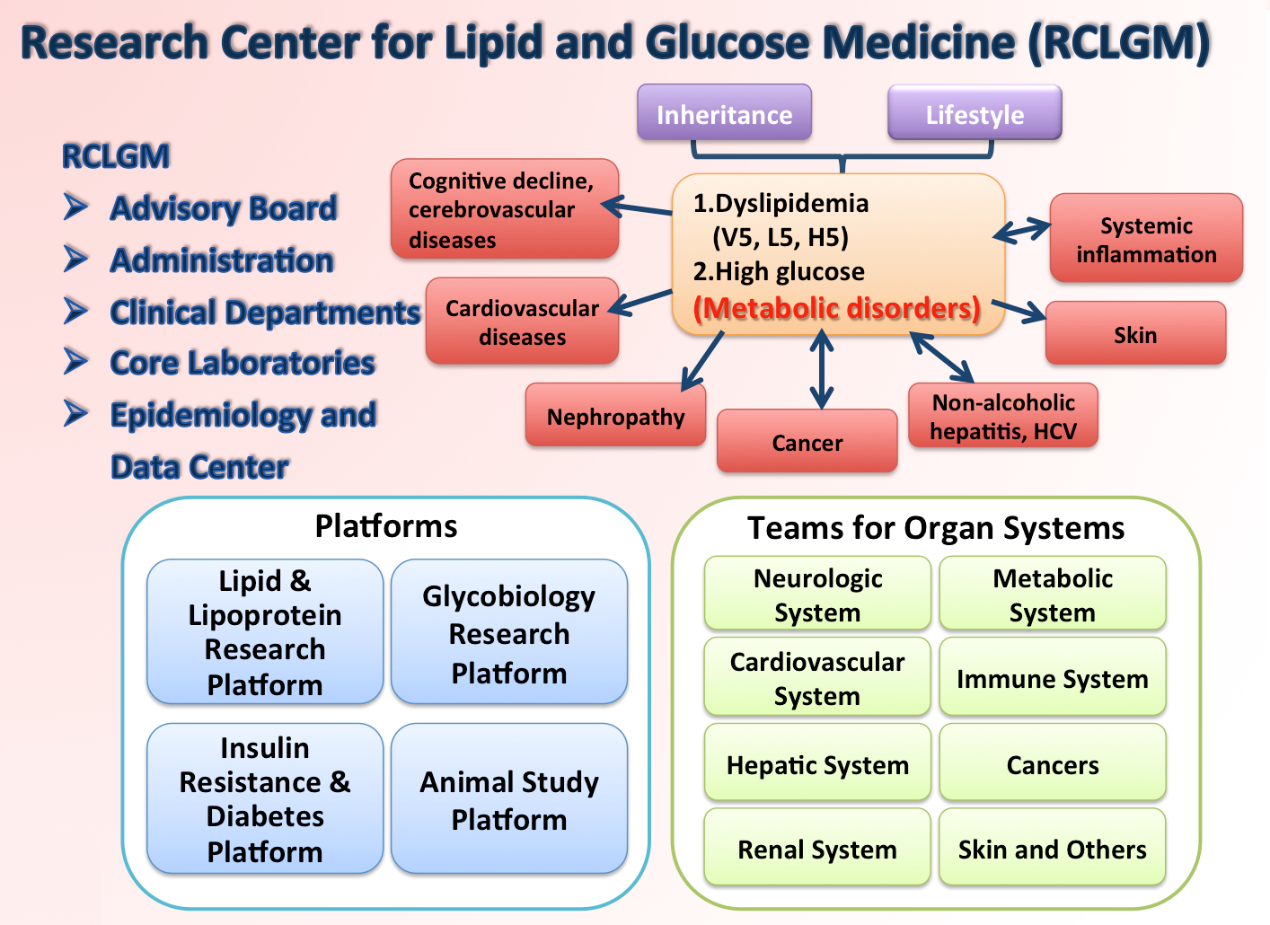
Ministry of Health and Welfare reported that the 10 leading causes of death in 2013 are malignancy, cardiovascular disease, cerebrovascular disease, diabetes, pneumonia, chronic pulmonary disease, accident, chronic liver disease and liver cirrhosis, hypertension-related disease, nephritis and nephropathy in our country. Dyslipidemia, diabetes and hypertension are the most important risk factors for these diseases, particularly for cardiovascular disease, cerebrovascular disease, chronic kidney disease (CKD), non-alcoholic fatty liver disease(NAFLD) and chronic systemic inflammation. Additionally, emerging evidence strongly suggests that lipoprotein aberrations and diabetes also play an important role in cancer formation, cognitive impairment, some infectious diseases, and premature senescence of stem cells. On the contrary, cancer, these infectious and even autoimmune diseases have also been found to result in lipid abnormalities and glucose intolerance. With the increasing prevalence of obesity and metabolic syndrome in Taiwan, it is of utmost urgency to launch a carefully orchestrated campaign against the formidable abnormal lipids and glucose intolerance. In response to this calling, we propose to establish a multi-institutional Research Center for Lipid and Glucose Medicine to investigate comprehensively the etiology, biochemistry, molecular biology, functionality, epidemiology, and clinical impact of abnormal LDL, VLDL, HDL and glucose entities in the Taiwan population.
- Dyslipidemia — A quality rather than a quantity issue:
Up to date, most clinical lipidology studies in the world are still focused on the efforts of lowering LDL cholesterol (LDL-C) and raising HDL-C concentrations in the plasma. However, effective lowering of LDL-C with the most potent statins does not preclude the occurrence of acute myocardial infarction; elevation of HDL-C with cholesteryl ester transfer protein inhibitors or niacin failed to prove clinically beneficial, and in fact may even be harmful. This paradox may stem from the negligence over the structural and functional heterogeneity among the particles within each lipoprotein class. - A new concept — Charge-defined VLDL and LDL subfractions:
In searching of atherogenic LDLs, most researchers subdivide LDL according to the particle size and density. Through such efforts, the abundance of a subclass designated as the “small, dense LDL” has been found to be correlated with the presence and clinical manifestations of atherosclerosis. However, so far small-dense LDL particles have yet to be retrieved from human plasma for mechanistic scrutiny. We have resolved human plasma LDL and VLDL into 5 electrical charge-defined subfractions (L1-L5, V1-V5) by anion-exchange chromatography. Unlike the density and size-oriented LDL entities classified by nuclear magnetic resonance, the chromatographically resolved L1-L5 LDL particles can be easily retrieved for further chemical and functional characterization. In a series of publications, we have demonstrated that L5, the most electronegative LDL subfraction, exclusively among L1-L5, exhibits potent atherogenicity in both in vitro and in vivo settings. The functionality of L5 is determined by its underlying chemical properties defined by us. Using the same technology, we have also divided HDL into H1-H5 subfractions. Compared with H1-H4, the most electronegative H5 exhibited the least capacity of performing reverse cholesterol transport (RCT), the primary anti-atherosclerotic function of HDL. In addition to their conventional roles in vascular biology, both VLDL, LDL and HDL are the most important “carriers” of proteins, cholesterols, and lipids to and from cells in different parts of the body. As naturally occurring nanoparticles, V5 and L5 may induce adverse biological reactions in multiple organ systems. - Etiologies of diabetes and its complications are not unraveled:
Type 2 diabetes is one heterogeneous disease. Thousands of genetic investigations have only demonstrated a weak association of some gene SNPs with the development of type 2 diabetes and its complications. We have published many reports in which patients with hepatitis C have higher prevalence of DM development, higher proportion of patients with poor glycemic control. More recently, we find out one gene, DM-related hepatic gene A, is associated with the development of type 2 diabetes. Several molecular mechanisms for diabetic complications have been mentioned, but no beneficial prevention has been reported from the huge amount of studies. Therefore, novel pathophysiological mechanisms are needed to unravel. In our unpublished experiments, high glucose impair RBP4-STRA6 binding by inducing the O-GlcNAcylation of STRA6; and then activate apoptosis, inflammation and fibrosis. Vascular senescence has recently been reported to involve in endothelial dysfunction and atheroscerosis. We reasonably assume that high glucose will cause vascular senescence via STRA6.CRBP1/RARα. Fenretinide, RBP4 inhibitor, can reduce obesity and glucose intolerance. Thereafter, we wish to investigate whether fenretinide can reverse inflammation, senescence and prevent diabetic complication. Additionally, the effect of Steep4-inducing agents on the prevention of diabetic nephropathy is worthy investigating. UKPDS and DCCT showed that legacy effect, or so-called metabolic memory, exist in diabetic patients. The mechanism is worthy studying when we hypothesize that O-GlcNAc transferase and Ten-Eleven translocation proteins may play an important role.
Missions
Research, Education, and Service.