脂質科學
脂質被認為是可以調節細胞過程的關鍵介質,並可能誘導多種信號通路。此外,使用脂質代謝物作為細胞生物標誌物可以指示不同的生物狀態和細胞活動。細胞中脂質的總含量就是脂質組。細胞脂質組中的任何修飾都會誘導或調節與細胞功能相關的信號傳導。
根據報導,包括極低、中度和低密度脂蛋白(VLDL、IDL 和 LDL)顆粒在內的脂質代謝物與心血管疾病如心肌梗塞(MI)和缺血性中風 (IS) 呈正相關。相比之下,高密度脂蛋白 (HDL) 顆粒已被證明與心肌梗塞死亡的發生呈負相關。脂肪細胞形成的過程,也稱為脂肪生成,受複雜分子過程網絡的調節,這種調節機制也可能受到脂蛋白的影響。因此,我們假設脂蛋白調節分化為心肌細胞和內皮細胞,從而影響心臟組織功能和再生。脂蛋白包括膽固醇、三酸甘油脂和磷脂。這些血脂是脂溶性的,必須與血漿蛋白結合形成脂蛋白,才能通過血液輸送到各個器官和組織。
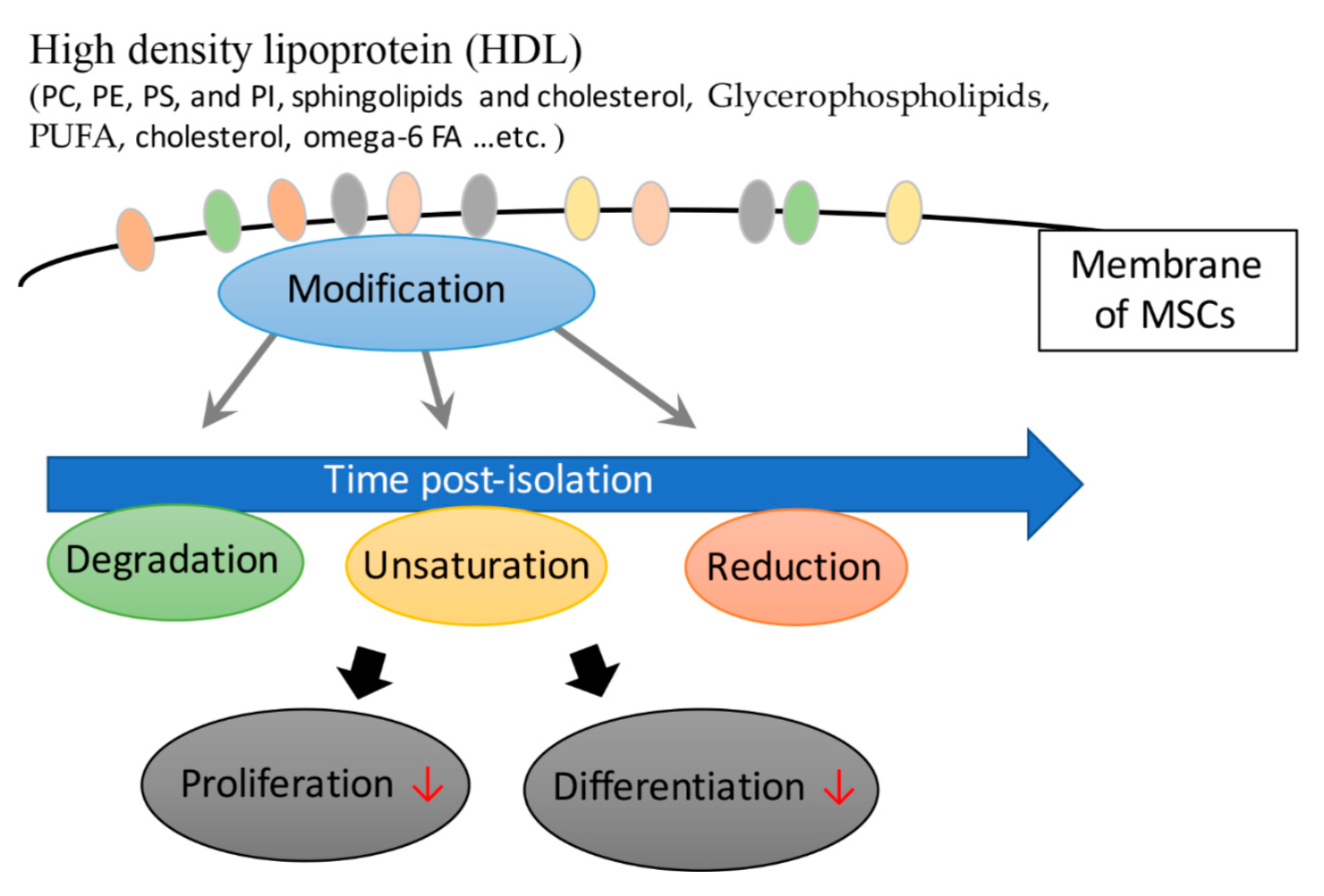
高密度脂蛋白 (HDL)
血液中總共有 20-30% 的血漿是由高密度脂蛋白轉運的,主要是將周圍組織的血漿帶回進行胰島素代謝。一個人的高密度脂蛋白水平越高,罹患冠心病的機會就越低,因此高密度脂蛋白膽固醇被稱為“好”的血漿。HDL的主要含量是磷脂,包括磷脂酰膽鹼(PC)、磷脂酰乙醇胺(PE)、磷脂酰絲氨酸(PS)和磷脂酰肌醇(PI)。鞘脂和膽固醇主要用作膜和細胞器的組成部分。在源自人類胎膜 (hFM-MSCs) 的間充質基質細胞的成熟階段,含有多不飽和脂肪酸 (PUFA) 的脂質種類增加。 Chatgilialoglu 等人發現在體外培養 hFM-MSCs 會改變它們的脂肪酸組成。為了維持和改善 hFM-MSCs 的功能特性,量身訂製的脂質補充劑可以模擬與其生理對應物相似的膜環境。幹細胞也可用於患者以達到治療效果。結果還表明,磷脂與間充質基質細胞分化之間存在關聯。
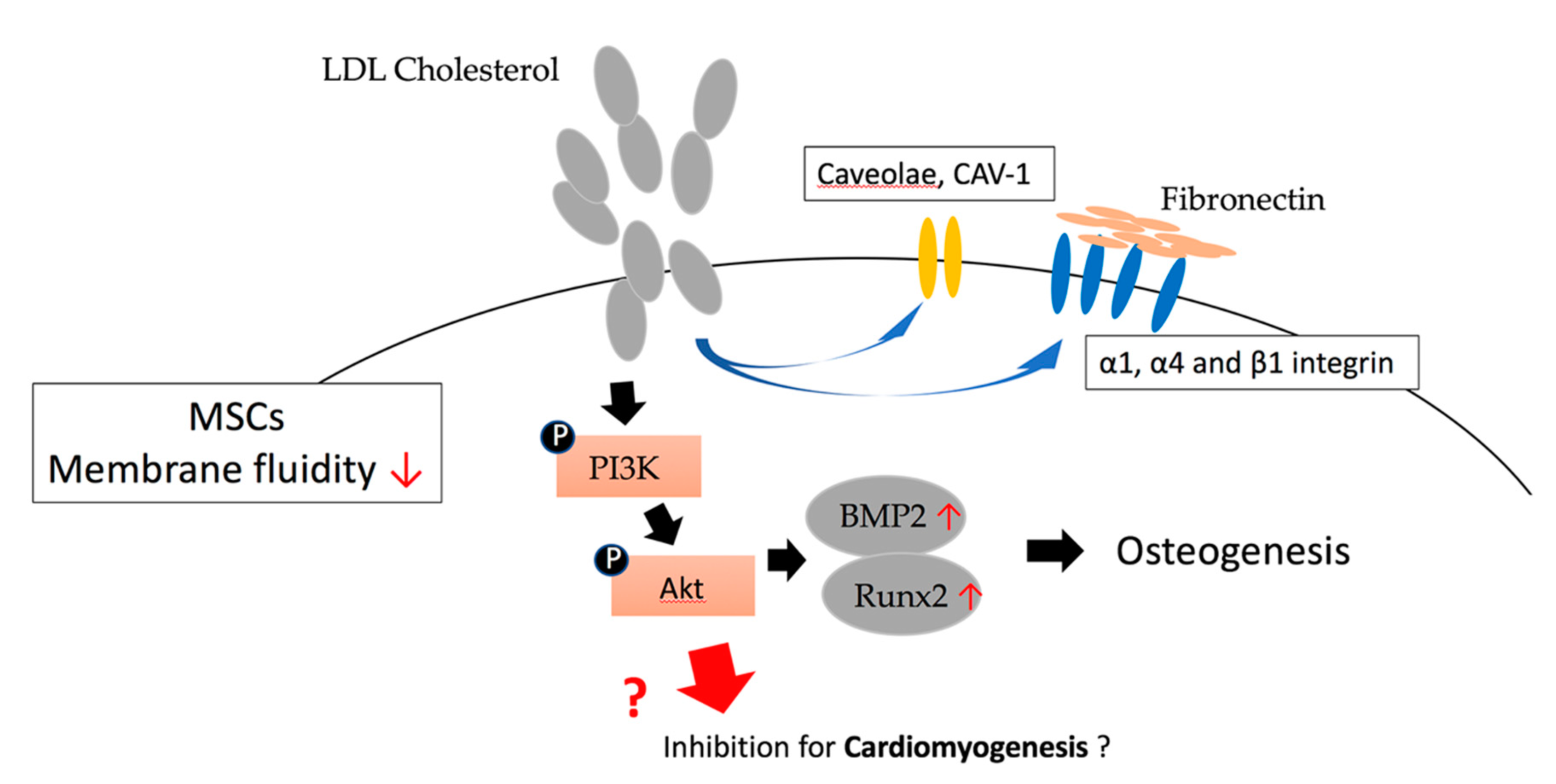
血液中 60% 到 70% 的膽固醇是由低密度脂蛋白攜帶,主要是將膽固醇從肝臟帶到周圍組織。低密度脂蛋白膽固醇過多引起的高膽固醇血症是冠狀動脈粥狀硬化和心臟病的危險因素,因此低密度脂蛋白膽固醇被稱為“壞”的膽固醇。越來越多的證據支持這一個觀點,即脂質/脂蛋白會對心臟組織(包括心肌、瓣膜和血管)產生脂毒性。根據報導,低密度脂蛋白 (LDL) 在誘發動脈粥狀硬化疾病以及在慢性炎症性疾病中發揮具有細胞毒性作用。已知最典型的氧化低密度脂蛋白 (oxLDL) 與冠狀動脈疾病 (CAD) 有相當大的關係。帶陰電性的低密度脂蛋白可分為五個亞型,從L1到L5,都表現出血管細胞促進動脈粥狀硬化形成的能力。其中,在患者血漿的 LDL 中攜帶最強陰電性的 L5 被發現與心血管疾病風險增加有關,與吸煙、高膽固醇血症、第 2 型糖尿病和代謝症候群的風險相當。與L1相比,L5含有較高的總蛋白和三酸甘油脂,但膽固醇酯相對較少,表明L5的脂毒性通過細胞過程激活相關的各種粘附分子和趨化因子。凝集素樣氧化的 LDL 受體-1 (LOX-1) 已被證明對帶陰電性的配體具有高結合親和力,這有助於下游信號傳導,例如 Bcl-2 家族,從而導致細胞死亡。仍在研究 LDL 和 L5-LDL 與冠狀動脈疾病 (CAD) 風險的關係,以及這些脂蛋白如何影響相關組織和細胞的機制。
極低密度脂蛋白 (VLDL)
我們還報導了極低密度脂蛋白 (VLDL) 可分為五種不同類型,由陰電性定義,稱為 V1 至 V5,具有不同的生物學功能。我們發現 V5 在患者血漿中的所有 VLDL 中表現出最大程度的細胞毒性,並且代謝症候群患者血漿中 VLDL 的百分比高於正常人。代謝症候群 (MetS) 患者的 V5/VLDL 百分比和濃度顯著高於正常人群。富含 V5 的 VLDL 異常高含量可能會增加罹患糖尿病、相關血管病變和心肌病的風險。血脂異常很容易與心房顫動(AF)相關,心房顫動可能源於多種心血管疾病,包括心力衰竭、高血壓、心肌梗塞、瓣膜性心臟病和風濕性心臟病。我們已經證明,與接受治療的小鼠中的正常 VLDL 相比,MetS 患者的 VLDL (msVLDL) 可導致顯著的左心房擴大,同時射血分數降低,並伴有老年 msVLDL 小鼠的無端心房顫動。我們的證據表明 VLDL 在心肌細胞和心房顫動發病機制中的關鍵細胞毒性作用。這些數據表明 VLDL 和 LDL 對人體組織,尤其是心臟組織的潛在毒性,這可能與心臟病的發生有關。